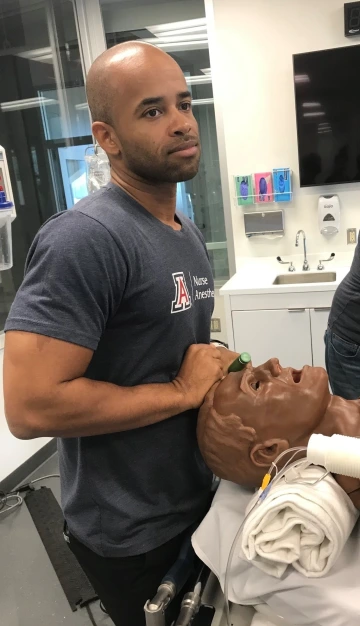
Catching up with DNP Nurse Anesthesia Student James Gibson

When we first profiled University of Arizona College of Nursing Doctor of Nursing Practice (DNP) nurse anesthesia student James Gibson in June 2020, he was neck-deep in the throes of the COVID-19 crisis. He had yet to begin his clinical training and was working nights as a registered nurse in a Veteran’s Administration COVID Intensive Care Unit in his native Southern California. Gibson battled anxiety, fatigue, and uncertainty daily, but he never lost sight of his goal of furthering his knowledge, life experience, and education.
Now only a few months away from May convocation, Gibson is finishing up his post-doctoral work, completing his clinical training and planning for the future. Despite the difficulties of the past two years, as he tackles the intensive final stretch of his studies, he is optimistic, driven and eager for new challenges.
“Choosing to pursue nurse anesthesia at the University of Arizona was one of the most difficult decisions that I made, but it turned out to be one of the best decisions. It is really like a family environment," ~ James Gibson, DNP nurse anesthesia student
What have you been up to since 2020?
I’m finishing up my post doc work and my clinicals, basically putting into practice what we’ve learned. It’s been very challenging because there’s a steep learning curve. As an ICU nurse you’re sharp at the skills that you do, but in the clinical setting you’re pretty much starting from scratch and learning new skills. I did most of my training in Southern California but after nine months I got the opportunity to go to a clinical site in South Texas.
Have your feelings about frontline health care work changed as the pandemic has evolved?
In the beginning, it was a scary time. You didn’t know what would happen if you got it, how to treat it, or how it would affect your family if you gave it them. We’ve had multiple surges since then and there’s definitely a lot less fear now, especially with the vaccine. I actually caught COVID for the first time last week, which wasn’t scary at all. It was just more of a hassle because I had to miss work and clinicals. That’s a stark contrast to a year and half ago.
Have you experienced issues with burnout?
Last year at this time was really tough, working in the hospital as an ICU nurse. You’d go to work to be with really sick patients, and when you’d come back, those patients would be gone. Normally, for an ICU nurse, the patients don’t die too often. But going to work every day where you have to do CPR on a patient because they’re crashing, and at the same time being in the midst of trying to protect yourself – it’s hard. So many things are going on that you don’t even have time to process it.
Has all this changed your thoughts on the importance of the nurse anesthesia field?
It made me realize just how important what we do is and how valuable we are to the health care system. During those peak surges, a lot of times elective surgeries are cancelled, which is the bread and butter of our work. Even still, CRNAs were able to transition to ICUs to do COVID interventions like breathing tubes, central lines so patients can get the medications to help keep them alive, and arterial lines to monitor their blood pressure. We were able to take our very important set of skills and use them in the ICU. It’s helped me realize how important we are and how essential it is to work as a team, whether you’re an ICU nurse, or a Nurse Anesthetist.
What are your post-graduation plans?
Last Monday I went on an interview in a small town in Northern California. I’m from southern California, so that was a big change. But the fact that CRNAs practice independently there piqued my interest. When I did the interview, the thing that really sold me was that it’s a supportive place where the people love their jobs and will give me the opportunity to grow in the best environment. When I thought about it, I decided to take the job. It’s scary and also exciting, but I’m looking forward to the challenge and to utilizing all the great things that the faculty at the University of Arizona taught us.
What’s your biggest takeaways from the CRNA program?
Choosing to pursue nurse anesthesia at the University of Arizona was one of the most difficult decisions that I made, but it turned out to be one of the best decisions. It is really like a family environment. Since my time in the program, I’ve helped mentor at least three other people who have gotten into the cohort specialty. In 2020 I was mentoring a co-worker with preparing for the program. He got an interview and then he was put on the wait list, and then in January of 2021, he told me that he had he had a rare form of cancer and it was really bad. He also told me that he was accepted into the UArizona Nursing CRNA program. He said “We did it.” And I told him “No, you did it. I just gave you the blueprint.” That day I called Dr. Kristie Hoch, our program director, and told her about what had happened and how worried he was about not being able to start the program because of his diagnosis. She said she would talk to him and that she’d save him a spot for next year so he could get better. You don’t normally get that from a program director. That just meant so much to him, that sense of being part of a family environment. But unfortunately, he passed away six months later.
What advice do you have for students thinking of following in your academic footsteps?
I’ve spoken to the DNP One’s -- the cohort that just got in last year -- and I’ve told them, “You’ve got to take advantage of this opportunity, because there are people who work so hard to be in your shoes and unfortunately they didn’t have the opportunity. You have to really think twice before you complain about certain things that aren’t really important, because you have an opportunity here that people have died in pursuit of.” Don’t take it for granted. It’s an opportunity to make a dream become reality. Be grateful. You don’t have to do this. You get to do this.

